
The Centers for Medicare and Medicaid Services has updated the Five-Star Quality Rating System, causing significant movement in nursing home domain ratings.
While some nursing homes may have missed the announcement about Centers for Medicare and Medicaid Services (CMS) updating the Five-Star Quality Rating System methodology beginning April 1, it would be difficult to ignore it now. With the recent release of CMS’ Nursing Home Compare quarterly data, the full impact of these updates can now be assessed.
Since the changes have taken effect, we have analyzed swings within specific domains as nursing home ratings rise and drop based on the new criteria. By highlighting some of these swings, we can better evaluate the cumulative impact of CMS’ updates.
CMS star rating changes effective April 1
CMS made key changes to the Five-Star Quality Rating program, including updates to these domains:
- Health inspections domain. In 2017, CMS implemented a new inspections process. During the transition, CMS temporarily held constant (or froze) the health inspection star rating for nursing homes for roughly a year. The agency decided to end the freeze on health inspection star ratings and resume the traditional method of calculating these scores by using three cycles of inspections. Inspections occurring on or after November 28, 2017, are included in each facility’s star rating. Additionally, in a separate memorandum, CMS provided new guidance to state surveyors on “immediate jeopardy” findings. While the guidance goes beyond nursing homes to cover all Medicare and Medicaid entities, it is still relevant for star quality ratings.
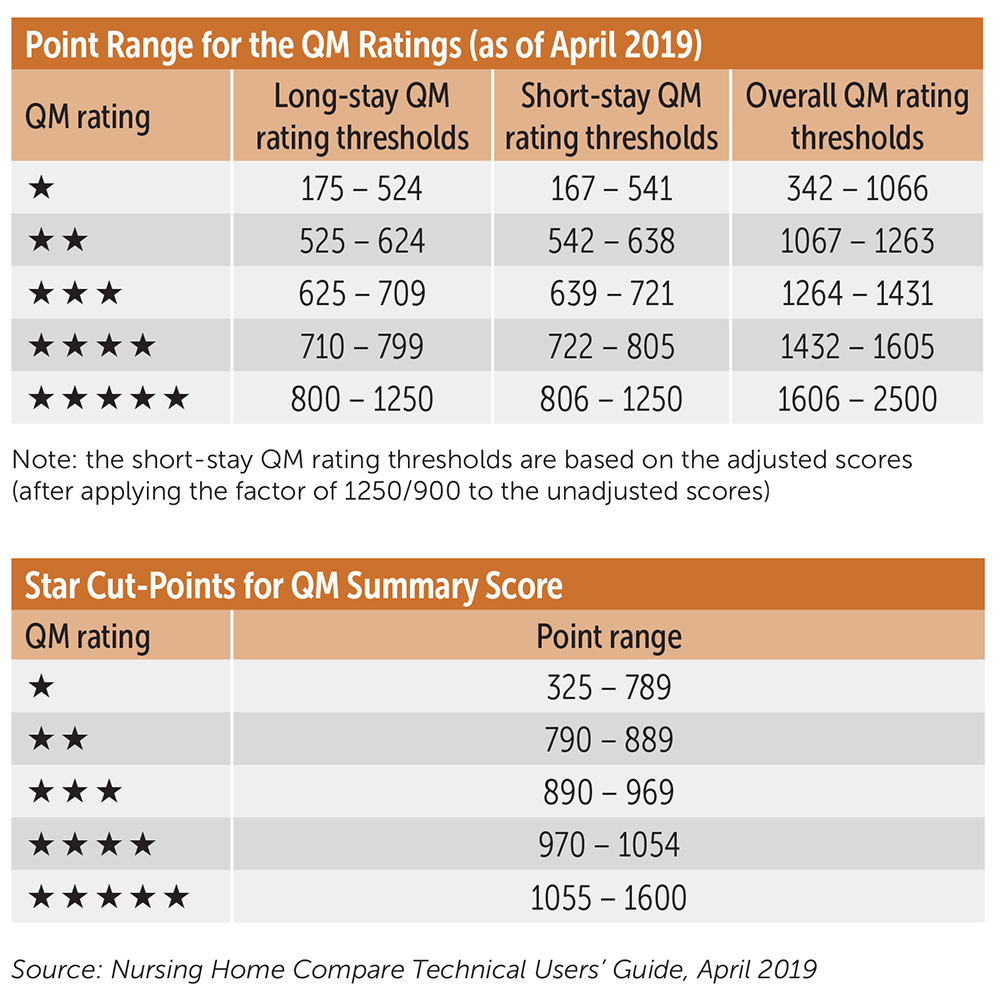
- Quality measure domain. CMS made multiple changes to the quality measures (QM) domain. The agency will use a separate measure rating for short or long stays to reflect the level of quality provided for these two subpopulations in nursing homes. Thresholds for ratings will be updated every six months, as well as weighting and scoring individual QMs differently. CMS is also adding a long-stay hospitalization measure and a long-stay emergency department (ED) transfer measure to the rating system, among several other measure changes.
- Staffing domain. CMS made a key change to the staffing domain with respect to the number of days without a registered nurse (RN) on site. The previous requirement began in 2018 and uses Payroll Journal Reporting (PBJ) for a more accurate look at facility staffing requirements. Previously, a facility with no RN on site for seven days or more received an automatic downgrade to one star in the staffing domain rating. CMS lowered the threshold from seven to four days.
Overall impact of star ratings on nursing homes
The overall impact of these changes resulted in considerable shifting within the star ratings for skilled nursing facilities (SNFs). Using CLA Clarity to dissect the impact of these changes, we found a total of 7,937 nursing homes’ ratings were positively or negatively impacted. Under the new methodology, 2,387 nursing homes increased their ratings by one or more stars, while 5,550 lost at least one or more stars. Overall, 53 percent of all facilities’ stars ratings were impacted under the new change.
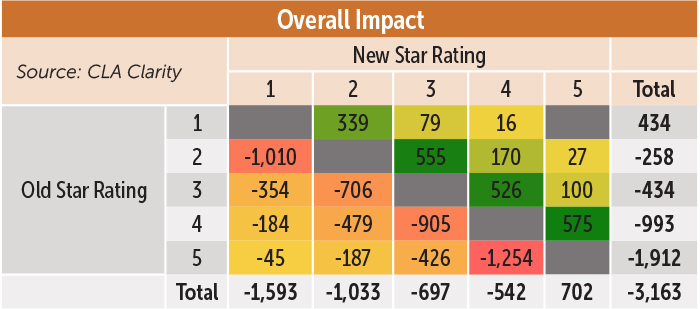
Following CMS’ changes, 1,159 additional facilities dropped to the lowest ranking of one star. In addition, 1,210 fewer facilities held the highest ranking of five stars. However, these changes have resulted in a more even distribution of facilities among the stars.
| Star rating | Previous percent of facilities | New percent of facilities |
|---|---|---|
| Five-star | 29% | 21% |
| Four-star | 23% | 22% |
| Three-star | 17% | 19% |
| Two-star | 20% | 19% |
| One-star | 12% | 19% |
Our analysis reveals the largest impacts were to the top and bottom ratings, where there were fewer five-star facilities and more one-star facilities. Quality and staffing domain changes drove the redistributions. Cory Rutledge, Principal, CLA
Star ratings impact by domain
By looking into the domains, we can better understand which changes had the largest impact. The data shows that quality domain had the most significant impact on ratings, followed by the staffing domain, and then health inspections.
QM domain. Overall, changes to the quality domain resulted in a net of 7,265 facilities losing at least one star. The largest jumps were 2,298 five-star ratings falling to a four-star, which also caused many facilities to lose the positive +1 quality bonus. Additionally, 2,359 previously five or four-star ratings dropped to a three-star. A total 2,314 facilities dropped at least two stars. On the positive side, 1,098 facilities moved up at least one star.

The new QM thresholds (listed below) used higher cut points than in the past, resulting in ratings decline.
Staffing domain improvements. CMS continues to be focused on staffing as a key element in nursing home quality and safety. CMS adjusted the threshold related to the number of days without a registered nurse (RN) on site from seven days to four days without it impacting the staffing domain rating. If no RN is on site for more than four days, it results in an automatic downgrade to one star in the staffing domain.
In a subsequent blog post about nursing homes, CMS Administrator Seema Verma highlighted the importance of staffing to the agency.
CMS has long identified staffing as one of the vital components of a nursing home’s ability to provide quality care. CMS collects staffing data from nursing facilities through the PBJ system based on payroll and other verifiable and auditable data, as required by law. Since November 2018, CMS has shared this data with SSAs [State Survey Agencies] so they know which nursing homes may have potential staffing problems and can target their reviews. SSAs are conducting a portion of their unannounced after-hours and weekend inspections to focus on staffing problems during those times.
In looking at the changes within the staffing domain under the new four-day threshold, we can see 5,066 facilities that dropped at least one star rating. The largest drops were 1,597 facilities that dropped from three stars to two stars, and 1,717 facilities that dropped from four stars to three stars.
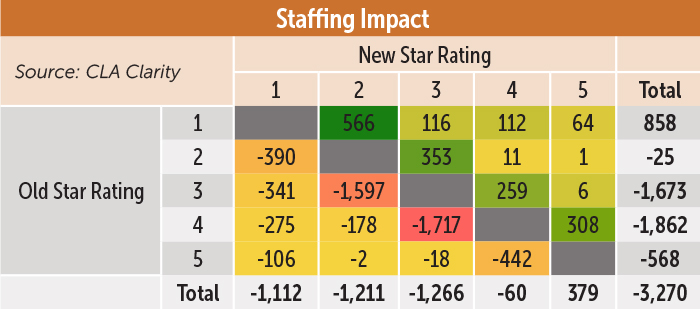
The largest positive improvements were 566 facilities that moved from a one-star rating to a two-star rating. In total, 1,806 facilities moved up in their star rating under this domain, of which 310 moved up at least two stars.
Health inspections. Overall, there was a net positive movement of 210 facilities due to survey impact changes. This was the only domain to see a net improvement. That being said, there was considerable movement within the ratings themselves, with thousands of facilities gaining or losing stars. For example, 642 formerly two-star facilities moved to one-star, 774 three-star facilities moved to a two-star, 780 four-star facilities moved to a three-star, and 538 five-star facilities were downgraded to a four-star. A total of 1,007 facilities went down at least two stars under this domain.
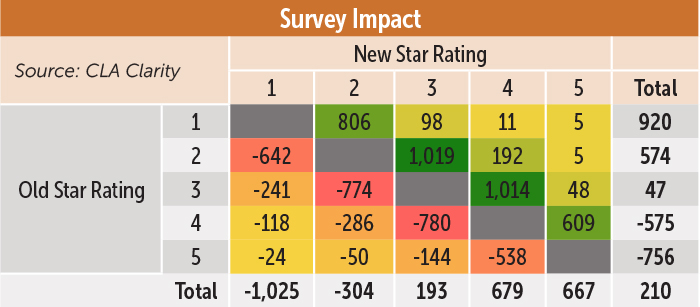
On the flip side, 806 previously one-star facilities rose to a two-star, 1,019 two-star to a three-star, 1,014 three-star to a four-star, and 609 four-star to a five-star. A total of 359 facilities rose at least two stars.
Low star ratings could result in reduced operating metrics
These updates reflect CMS’ continued push towards higher quality and patient safety in nursing homes. To account for these changes, facilities will need to re-examine their quality programs and their RN staffing models. Failing to adjust to these changes will not only impact star ratings, but can also introduce other long-term market obstacles such as inability to access sufficient capital, decreasing volumes, and declining margins.
Obviously, low star ratings are suboptimal for a variety of reasons, but one item worthy of note is that low ratings may preclude these entities from fully participating in value-based models. All providers, including nursing homes, unable to demonstrate what CMS believes are minimum levels of quality or cost efficiency will be increasingly marginalized in health care’s transition to value. Rob Schile, Principal, CLA
Our analysis shows strong correlations between CMS Five-Star Rating and key performance indicators, such as occupancy and Medicare volumes. Having a one-star rating publicly posted on Nursing Home Compare for staffing levels may result in consumers or referral sources bypassing a facility in favor of one with higher star ratings in this domain.
Lower star ratings also have the potential to limit full participation in value-based models. New staffing domain changes could lead to a facility’s overall star rating falling below three stars at a time when a three-star rating continues to grow in importance under Medicare. For example, only nursing homes with a three-star rating or above are eligible for a waiver of Medicare’s three-day inpatient hospital stay requirement under Medicare’s Accountable Care Organizations (ACOs). According to CMS data for 2018, 10 million Medicare beneficiaries are in ACOs. There are similar waiver requirements under other CMS bundled payment models.
Further, various value-based models allow for the creation of preferred provider networks for post-acute care. Star ratings, quality, and staffing are certainly aspects that will be assessed by ACOs or other conveners as they establish these preferred networks. If a nursing home does not have a higher star rating, it could very well be bypassed.
“The time is now for nursing homes to dig deep into changes occurring in the market and in Medicare, including new star ratings methodology and the forthcoming transition to the Patient-Driven Payment Model,” said Cory Rutledge, senior living leader with CLA.
How can CLA help
CLA is on top of the financial and regulatory changes impacting health care providers, including these Five-Star ratings changes, as well as modeling and preparing for the new Payment Driven Payment Model. Our senior living professionals can also help you model the financial impacts of changing star ratings.
