
Key insights
- CMS finalized additional codes and payment adjustments for chronic care management (CCM) and principal care management (PCM) while also adding remote therapeutic monitoring (RTM) to the mix.
- Complementary codes open the doors for improved transitional care management and behavioral health integration.
- A whole suite of care management codes, including new RTM codes, allows for even more robust care management in the future
Need help understanding the reimbursements surrounding care management codes?
According to the Centers for Disease Control and Prevention, six in 10 adults have one chronic condition and four in 10 have at least two chronic conditions. That means there is a significant amount of ongoing care management needed. In the final 2022 Physician Fee Schedule (PFS), the Centers for Medicare and Medicaid Services (CMS) demonstrated the agency’s support for care management by finalizing additional codes and payment adjustments for chronic care management (CCM) and principal care management (PCM) while also adding remote therapeutic monitoring to the mix.
There is now a suite of care management codes to consider — from CCM, PCM, and transitional care management (TCM) to behavioral health integration (BHI), remote physiologic monitoring (RPM), and newly created remote therapeutic monitoring (RTM).
But can these fit together to positively affect health outcomes and reimbursement? We’ll review some key codes and then look at a use case to show the potential reimbursements.
Code sets to keep on your radar
Chronic Care Management (CCM) and Complex CCM
CMS began reimbursing CCM codes back in 2015 and has regularly improved those codes, including under the 2022 final PFS rule. CCM requires an individual to have two or more chronic conditions that are expected to last for at least 12 months or cause death. If not addressed, the individual is at significant risk of death, acute exacerbation or decompensation, or functional decline. A comprehensive care plan must be established, implemented, revised, and monitored.
Per CMS, a few examples of chronic conditions include:
- Alzheimer’s disease and related dementia
- Arthritis (osteoarthritis and rheumatoid)
- Asthma
- Atrial fibrillation
- Autism spectrum disorders
- Cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Depression
- Diabetes
- Hypertension
- Infectious diseases such as HIV/AIDS
Under the 2022 PFS rule, CMS finalized an add-on code, 99437, to its existing CCM code set. The new code is used in conjunction with 99491 when a physician or qualified professional spends an additional 30 minutes on CCM activities.
With this addition, there are now four CCM codes and two Complex CCM codes. For Complex CCM, there are additional requirements, such as establishment or substantial revision of a comprehensive care plan; moderate or high complexity medical decision making; and 60 minutes of clinical staff time directed by a physician or other qualified health care professional, per calendar month.
Also in 2022, CMS increased reimbursements for all CCM codes to better reflect the time and resources used in managing these patients.

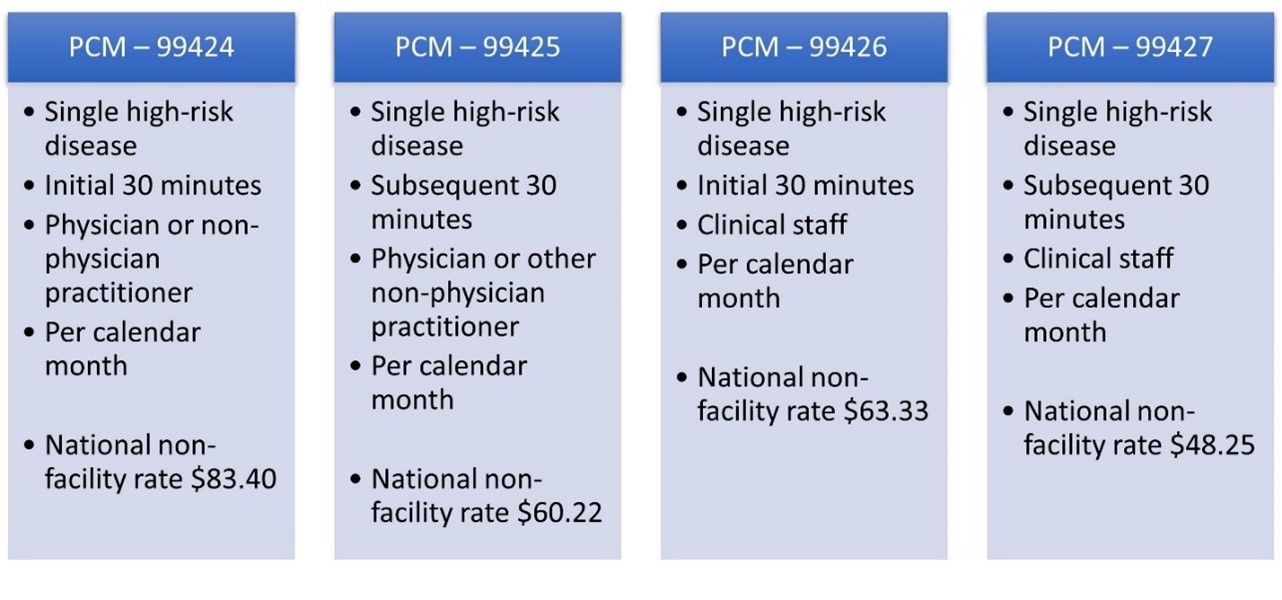
Principal Care Management (PCM)
Recognizing there are situations where patients have one chronic but serious condition, CMS finalized PCM in 2020. While CCM may pair well with primary care practices, PCM opens the door for specialists — such as cardiologists, gerontologists, oncologists, pulmonologists, or rheumatologists — who are managing a complex condition.
PCM requires that the complex, chronic condition last at least three months and is severe enough that failure to address it places the individual at risk of death, hospitalization (or had recently been hospitalized), functional decline, acute exacerbation, or decompensation. The condition requires the creation or revision of a disease-specific care plan. There is also the need for frequent medication adjustments and/or managing the condition is very complex due to comorbidities.
Under PCM, there are four codes available: two base codes depending on provider or clinical staff plus respective add-on codes for additional time spent. CMS also increased reimbursement for several PCM codes this year.
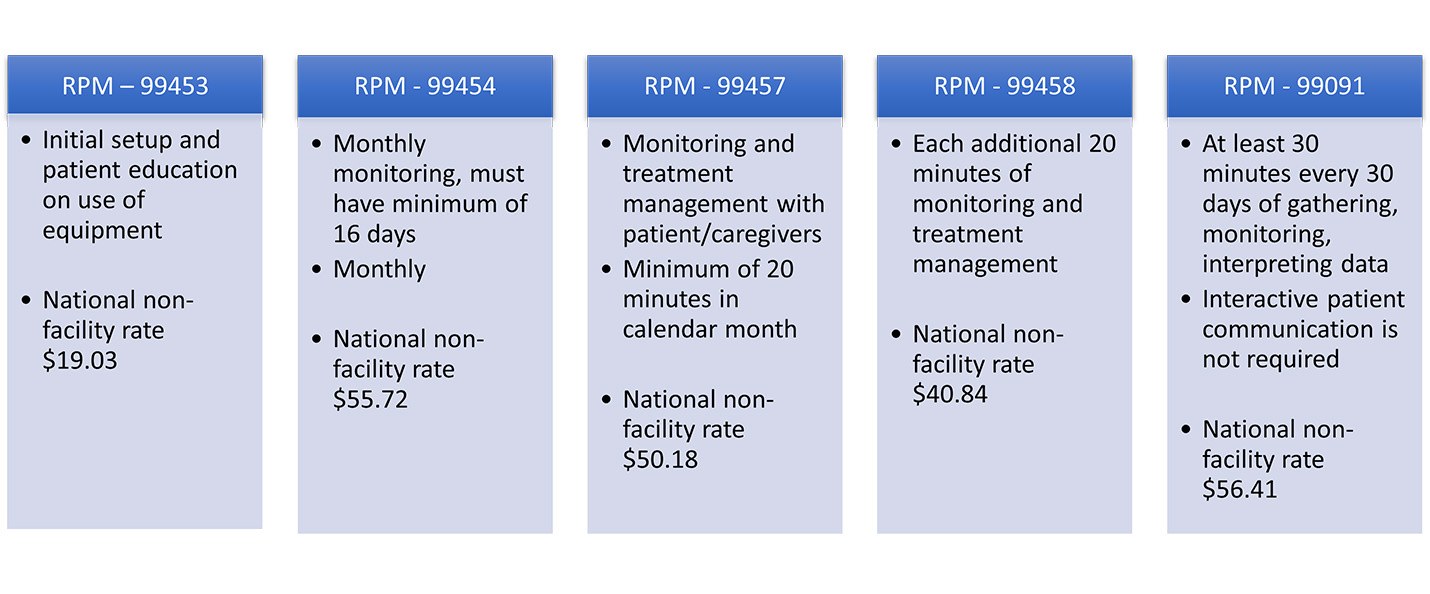
Remote Physiologic Monitoring (RPM)
When CMS finalized payment for RPM 2019, it showed that the agency recognized care management could be improved using technology. RPM is the remote monitoring of physiologic parameters such as weight, blood pressure, pulse oximetry, and respiratory flow rate. The code set allows for payment for the initial device setup and education, monthly transmission of data, plus reimbursement for managing or treating the patient’s condition when certain time limits are met each month.
A minimum of 16 days of data are required to bill monthly. The device setup and education code, 99453, may be billed only once. The RPM device must meet FDA definition but does not need to be FDA approved. Only one provider may bill RPM for a patient and reimbursement is irrespective of the number of peripherals or devices used.
There are many use cases, and RPM can be paired with other care management codes, like CCM. Of note, for 2022, CMS finalized lower reimbursements for the bulk of the RPM codes.
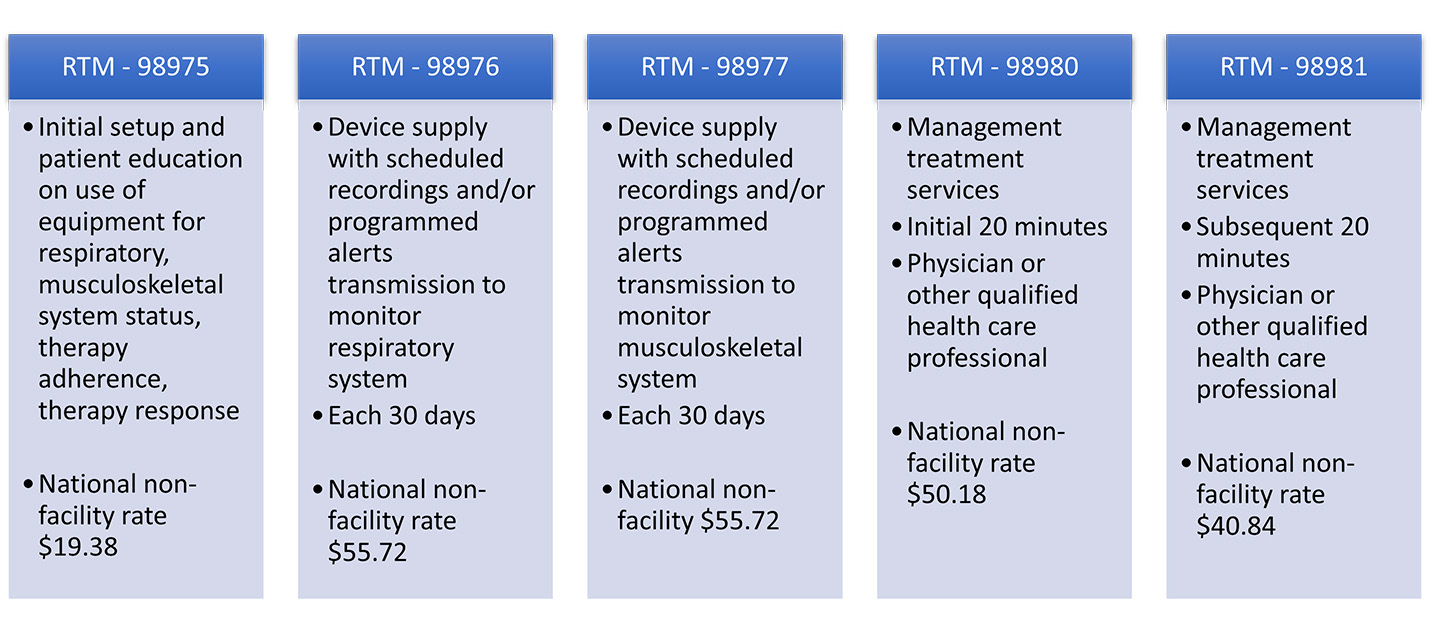
Remote Therapeutic Monitoring (RTM)
Building on the RPM code set, CMS unveiled five new codes related to RTM in 2022. RPM is for physiologic data whereas RTM includes non-physiologic and self-reported data on therapy adherence, therapy response, and monitoring respiratory and musculoskeletal systems. In a divergence from RPM, there are only two allowable device supply codes for RTM — one for respiratory device supply and one for musculoskeletal device supply — which will initially limit RTM’s use. The treatment and management codes are not as limiting.
Sample use case: Layering codes for enhanced care and reimbursement
Bill has chronic obstructive pulmonary disease (COPD), obesity, and co-occurring depression. He recently had a COPD exacerbation where he wound up in the ER and was ultimately admitted as an inpatient. He is being discharged to home. His primary care physician was alerted to his ER/inpatient admission and will handle his care management post-discharge.
The physician is concerned with Bill’s transition home, as he has several new medication changes and has expressed that his depression has worsened because of his recent hospitalization. The physician talks with Bill shortly after he is home via a telehealth visit. In this call and follow-up conversations with clinical staff over the next 30 days, discharge instructions are discussed with Bill and his wife, all his medications are reviewed, questions are answered, follow-up appointments are handled, and a comprehensive care plan is developed and implemented. His physician discusses using CCM and RPM. Bill agrees.
Bill’s physician initiates RPM. Bill receives his RPM devices at his home. Bill will use two RPM peripherals — pulse oximeter and spirometer — to monitor two key physiologic data for his COPD. A nurse from his primary care clinic educates Bill on the devices, helps him set it up and they test everything. Bill begins transmitting data. The physician’s clinical staff regularly review his RPM data, calling him whenever a flag triggers that data is moving out of expected ranges. The physician is involved as needed.
A nurse regularly checks in with Bill related to his medications, recovery, progress, and symptom management, including his depression. They also discuss his diet, nutrition, and exercise regimen. Bill’s physician believes pulmonary rehabilitation would be helpful and refers Bill to the local hospital’s program.
If questions or concerns arise outside of Bill’s normally scheduled check-ins, Bill calls his physician clinic to speak with his nurse or on-call provider (if after hours).
Bill’s physician periodically checks in with him virtually and has follow-up primary care visits as needed.
Over the course of the year, Bill does not go back to the hospital. He is participating in pulmonary rehab, which is helping him with his breathing exercises and nutritional choices, and his depression is well managed.
Financial model for Bill’s care
In our scenario, Bill is receiving TCM, CCM, and RPM from his primary care provider. TCM would only be billable once for the 30 days post-discharge. For TCM, Bill’s condition requires moderate complexity in medical decision making, which is reimbursed at a national non-facility rate of $209.02 for 2022.
Let’s assume he receives CCM and RPM for 12 months. For CCM, let’s assume his physician provides 30 minutes a month during the first three months post-discharge, as Bill’s medicines need to be regulated and his care plan is adjusted. The nurse provides 20 minutes for the remaining nine months.
With RPM, the device setup and education code is billed once with the transmission plus 20 minutes of monitoring/treatment each billed monthly for the year. Bill has virtual checks with his care team throughout the year. Let’s assume once per month.
| Chart 1: Bill Receives TCM, CCM, RPM, Virtual Check-Ins (Annual) | ||||
|---|---|---|---|---|
| Care management | Code | Amount | Frequency | Total |
| TCM | 99495 | $209.02 | Once | $209.02 |
| CCM | 99491 | $86.18 | 3 months | $258.54 |
| CCM | 99490 | $64.03 | 9 months | $576.27 |
| RPM | 99453 | $19.03 | Once | $19.03 |
| RPM | 99454 | $55.72 | 12 months | $668.64 |
| RPM | 99457 | $50.18 | 12 months | $602.16 |
| Virtual Check-in | G2012 | $14.54 | 12 visits | $174.48 |
| Total for Bill | $2,508.14 | |||
By documenting, separately tracking, and providing the required components of these codes, Bill’s physician and care providers could see a potential of $2,508.14 in reimbursement over the year for his care management alone.
Further, if the physician clinic had 500 patients like Bill, annual revenues for those patients could be more than $1.25 million. Even if we remove all the TCM and provide CCM/RPM/virtual check-ins only for those 500 patients, that still totals nearly $1.15 million annually (see Chart 2).
| Chart 2: 500 Patients Receiving CCM, RPM, Virtual Check-Ins (Annual) | ||||
|---|---|---|---|---|
| Care management | Code | Amount | Frequency | Total |
| CCM | 99491 | $86.18 | 3 months | $258.54 |
| CCM | 99490 | $64.03 | 9 months | $576.27 |
| RPM | 99453 | $19.03 | Once | $19.03 |
| RPM | 99454 | $55.72 | 12 months | $668.64 |
| RPM | 99457 | $50.18 | 12 months | $602.16 |
| Virtual Check-in | G2012 | $14.54 | 12 visits | $174.48 |
| Subtotal | $2,299.12 | |||
| Total 500 patients | $1,149,560 | |||
Looking to the future
This is only one of many potential use cases for care management coupled with technology and virtual care delivery. As we look to the future on these complementary codes, consider all the emerging opportunities. What about managing serious chronic mental illness through better primary care-behavioral health integration (BHI), which is currently reimbursable, and pairing that with smart pills to watch for therapy adherence? Consider a cancer patient whose oncologist is using PCM and the patient is taking an oral chemotherapy pill using either a smart pill or a smart pill bottle. And what if we could add a digital therapeutic, like a smart inhaler, for managing our earlier use case for Bill’s COPD?
If we look at other payment models — think Medicare Advantage, capitation, and value-based payments — care coordination, technology, and data analytics are foundational for success. These approaches look for unnecessary care, focus on preventive care, and use data analytics to analyze and stratify patients for improved care management. In the end, their goals are to keep people healthier within a pre-determined budget.
CMS continues to recognize the value and role of managing chronic conditions — whether highly complex, physical, or behavioral. We continue to see CMS evolving and refining these codes, which provide opportunities for better patient outcomes and needed reimbursement both now and into the future. CMS also cements its support for telehealth and other technology-based care options. Finally, CMS is looking to refine and realign the models it authorizes via the Innovation Center.
How we can help
Are you wondering how it can all work together and where you fit in? Have you assessed your patients to see if any could qualify for CCM, PCM, or RPM? Do you want to better understand the reimbursements surrounding care management codes and what that could look like for your practice? Curious about the future of payment models as they continue to unfold?
CLA’s health care regulatory, coding, and reimbursement teams can help you strategize, prioritize, and standardize your approach.
