
To move from traditional health care delivery models to population-focused models requires an understanding of the populations you serve.
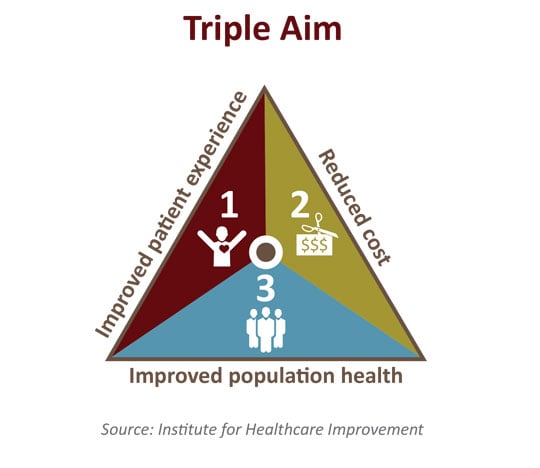
Many organizations are focused on developing and implementing population health management strategies within a reimbursement framework that still rewards volume. As health care delivery models are redesigned to fundamentally deliver care differently, health care institutions need a well-articulated plan to move from volume to value in order to achieve triple aim objectives (improving the health of the population, improving the experience and outcomes of the patient, and reducing the cost of care).
Separate patients into risk categories
Population health management requires bringing a new discipline to the delivery of health care. To make the transition from traditional delivery models to population-focused models, you need to understand the populations you serve and build a scalable approach. The first step is to segment patients into three risk categories. The next step is to focus on high-impact care priorities that yield the most value for each population segment.
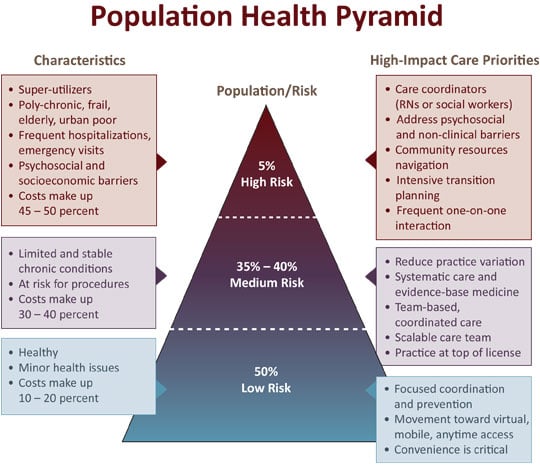
High risk patients are super-utilizers
The very sick patients at the top of the pyramid represent the super-utilizers of the population. These few patients typically account for upwards of 45 – 50 percent of the total cost of care in any organization. In the near term, the surest way to improve health care value while making it more cost effective is to recognize that high-risk patients typically have psychosocial and socioeconomic barriers that get in the way of managing their multiple chronic conditions. Finding ways to navigate these barriers will result in lower total cost of care and improved outcomes for this population. Using physicians to navigate complex non-clinical barriers is not a great use of a physician’s time or talent. Instead, look for opportunities to leverage social workers, RNs, and specially trained advance practice nursing partners to coordinate care and navigate community support for these patients. Frequent one-on-one interactions with high risk patients will yield the best opportunity to minimize re-admissions and limit high cost emergency visits.
Several approaches yield results for medium risk populations
Patients with moderately controlled or limited chronic disease such as diabetes, congestive heart failure, and cancer make up the middle of the pyramid. The best way to reduce total cost of care while improving patient experience and clinical outcomes is to focus on:
- Reducing practice variation by focusing on evidence-based medicine
- Developing physician-led care teams focused on innovation and patient-centered care
Physicians are best positioned to lead care teams made up of PAs, CNPs, RNs, pharmacists, social workers, and others. Dynamic care teams with clearly defined roles will have the opportunity to prevent progression to high-risk categories. Steadfast commitment to reducing practice variation and pursuing ongoing performance improvement yields the most value for medium risk patients.
Low risk and low cost
The 50 percent of patients who are generally healthy and have limited minor illness concerns account for less than 20 percent of the total health care spending of most organizations. These patients are looking for convenient and accessible care. Because the health care needs of this group are limited, it is unlikely that the expertise and skill of a physician is needed to effectively care for these patients. This population segment will become loyal customers by offering non-visit care opportunities such as phone, web advice, and automated reminders for prevention and screening services. Rethinking health care delivery and moving toward virtual, mobile, and anytime access will become increasingly important to this population.
How we can help
As the volume-to-value revolution continues, episodic, transactional care will be replaced with patient-focused interactions delivered by care teams intent on keeping populations healthy. Access is expected to become more virtual and convenient for lower-risk patients, thereby allowing more resources to be deployed to the super-utilizers. As health care institutions migrate toward population health care management strategies, they must design scalable solutions that can be adapted to changing patient needs. CLA can help your organization transform its care delivery model by identifying the high-risk, medium-risk, and low-risk patients and implementing appropriate care strategies for each population segment.
